Mental health: Taming the beast

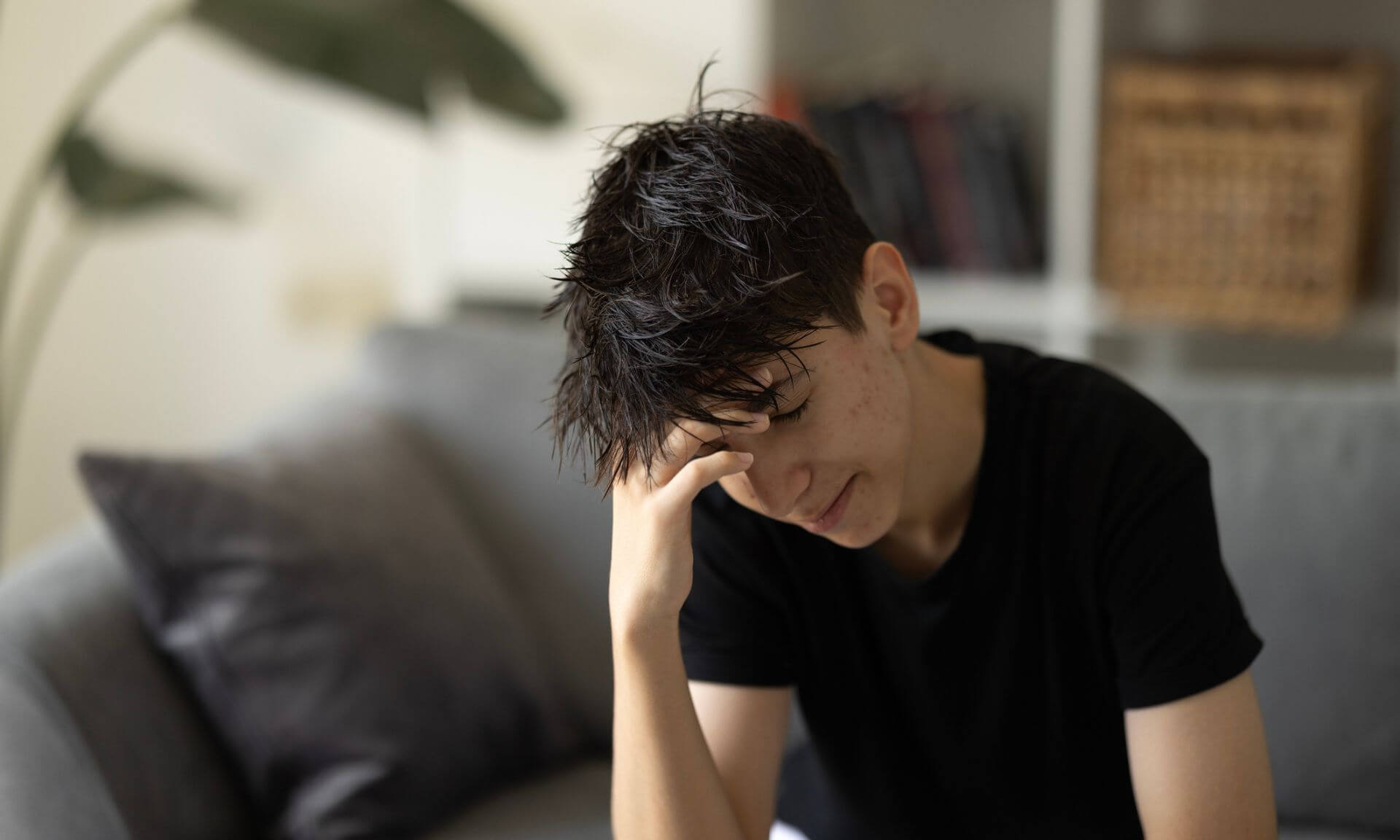
In 2019, as many as one out of every eight people worldwide were diagnosed with a mental disorder. By the following year, COVID-19 had crashed headlong into our lives and the numbers skyrocketed. More than one in four people suffers from major anxiety or depression – the two most common mental disorders – followed by bipolar, post-traumatic stress, behavioural, eating and neurodevelopmental disorders, and schizophrenia.
In Quebec, one in three patients who end up in the emergency room are struggling with a mental-health problem because they can’t access services or have no support network. But true recovery requires a long-term plan, according to Catherine Dugas, an occupational therapist and clinical lecturer at Université de Montréal’s School of Rehabilitation.
To navigate this new reality, future caregivers will need to draw deeply on their resolve, creativity and capacity to adapt – and UdeM's Faculty of Medicine is equipping the next generation of practitioners to respond to individual needs, without burning out in the process.
Finding meaning in what we do
The first thing these future doctors, psychiatrists and other health professionals will need to learn is how not to get discouraged navigating the lumbering behemoth that is our health system. And also how to keep their drive, passion and motivation intact.
An overhaul of UdeM’s medical program is currently underway, and with it the Faculty of Medicine is revisiting the notion of care, extending it beyond the technical and theoretical skills required. Just what role should physicians be playing in today’s world? How do we teach them to be good communicators? What should the doctor-patient relationship look like?
Clara Dallaire is a patient-partner and member of the Arts and Humanities communication subcommittee for the medical program review. She envisions “communication as a vast toolbox caregivers can harness to build trust with their patient, where their patient’s history, environment and personal resources are all factored into giving them the best care possible.”
The primal importance of self-care

Dr. Marie-Ève Goyer, associate clinical professor in the Department of Family and Emergency Medicine, warns new graduates not to run themselves to the ground just to meet performance indicators, as that can quickly lead to exhaustion.
“What we want is to provide quality care,” she said. “We want to feel that we are doing our job well and take the time to talk to our patients. It can be stressful working in a system like this. Needs are growing at an exponential rate. It’s up to us caregivers to know when to ease off, because nobody else can tell us. We have to learn to set our own limits, give ourselves the best possible resources and conditions in which to do our job creatively and with satisfaction.”
In other words, caregivers need to put a premium on their own mental health, be on the lookout for signs of burnout, and make sure they feel rewarded in their professional and personal lives.
Establishing priorities

Dr. Goyer is head of homelessness, addiction and mental-health services at the CIUSS Centre-Sud-de-l’île-de-Montréal (CCSMTL). She believes our health system has got it backwards: those who generally get the first crack at care are already in better health, because they’re well organized and have access to things like health insurance, a telephone and the internet.
“Imagine you’re living on the streets,” she said. “It’s -40 °C out there, and you’re in withdrawal. You should be first in line for care, but odds are, you won’t receive it. The question we need to ask ourselves as a society is, do we make taking care of our most vulnerable a priority?”
The Association des médecins psychiatres du Québec is working to clarify the responsibility psychiatrists have toward the populations they serve, and how to integrate it into their practice.
“Our future caregivers need to shift towards responding to needs rather than demands,” said Claire Gamache, the association’s president. “Because the people who most often seek psychiatric treatment are not necessarily the ones who need it most.”
Leadership and multidisciplinary teamwork

The health care system has limits, if we’re to have any chance of turning the ship around and providing people with better care, the next generation will have to step up and take the lead in developing new projects, the experts emphasize.
“It will take energy, organization, experience, knowledge and the skills they will learn as part of their training,” said Dr. Lison Gagné, a clinical professor in the Faculty of Medicine’s Department of Psychiatry and Addiction and the local psychiatry education coordinator at the CCSMTL.
“Our work in mental health is extremely demanding. We can’t be working in isolation. Psychiatrists need to be part of a multidisciplinary team: family physicians, occupational therapists, social workers, psychoeducators, psychologists, and therapists.
"They need to lead the way in supporting front-line workers and school staff. If they take care of their own mental health as they settle into this role, we’ll see fewer burnouts and fewer defections to private practice.”