Brain cancer: serious consequences for young survivors
- Salle de presse
03/28/2023
- UdeMNouvelles
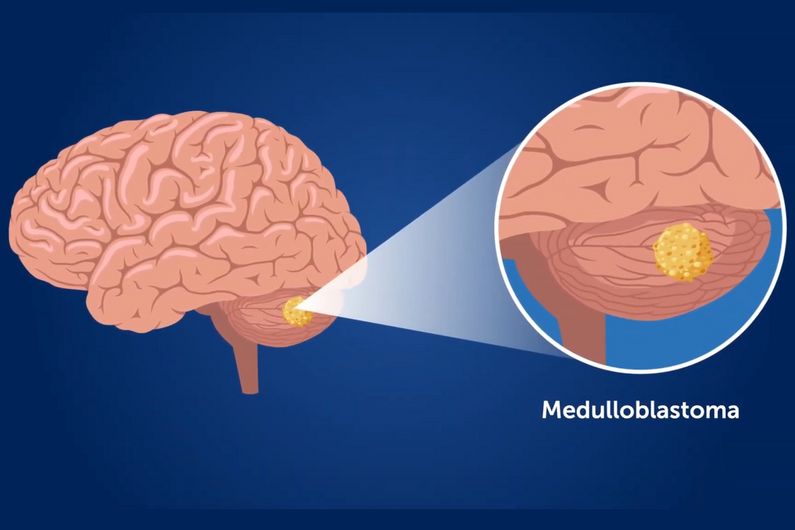
A new study shows the urgency of tailoring treatment regimens based on several criteria to provide better health outcomes for medulloblastoma patients.
From neurological problems to hearing loss and infertility, survivors of medulloblastoma, an aggressive form of brain cancer, are left with severe physical and cognitive impairments and have an overall mortality rate 21 times higher than the general population.
These findings are from a new study led by Dr. Hallie Coltin, a pediatric hematologist/oncologist and researcher at CHU Sainte-Justine and assistant clinical professor at Université de Montréal’s Faculty of Medicine.
Published in late January in the Journal of Clinical Oncology along with an editorial and a video,
these results highlight the urgent need to tailor treatment regimens based on age, disease severity, and tumor biology to improve health outcomes.
Medulloblastoma is the most common form of brain cancer in young people. Currently, the survival rate ranges from 50 to 80 per cent. However, available treatments for the disease are not without consequences. In this study, children under 18 years of age diagnosed with medulloblastoma and surviving for more than five years without recurrence have 45- and 96-fold higher rates of stroke and severe hearing loss, respectively, than the general population. In addition, about one in two patients receives disability assistance, a figure that Coltin believes is underestimated.
“In recent years, patients have survived medulloblastoma, but the late effects such as serious neurological and cognitive problems are likely reducing the chances of having a life partner and must be addressed,” said Coltin.
These findings suggest a need to review treatment regimens to include risk-stratified therapies based on age and tumor biology so patients at low risk of relapse are not exposed to toxic chemotherapy and radiation treatments. It’s also important to reduce the long-term burden of the disease and allow young medulloblastoma survivors to achieve optimal health and quality of life.
A sign of hope
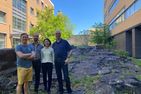
On the morning of his 16th birthday, Jonathan Roy-Ascanio—a patient of Dr. Sébastien Perreault, a neuro-oncologist at CHU Sainte-Justine—was given the devastating diagnosis of medulloblastoma following an extensive investigation and the results of an MRI scan. The medical team was very efficient and removed the brain tumour the same evening. This was followed by 11 months of life-saving targeted chemotherapy and radiation treatments.
With slight hearing loss and somewhat reduced ability to focus, Jonathan is now pursuing a bachelor’s degree in software engineering at UdeM. “I’d like to thank Dr. Perreault for allowing me to go to school even during my treatments and all the doctors and researchers who are making scientific advances to improve our life prospects and to mitigate the after-effects of the disease,” he said. “Their work is helping people like me return to a normal life.”
This case shows how optimized treatments can have major health benefits for patients.
Administrative health data from the province of Ontario associated with 230 medulloblastoma survivors under 18 years of age between 1987 and 2015 were compared with 1,150 healthy controls of similar age, sex and location. In this group, 81.3 per cent of patients received cranial and spinal radiotherapy. This work was necessary to get a clear picture of the situation and provide optimized treatments.
About the study
"The burden of surviving childhood medulloblastoma: a population-based, matched cohort study in Ontario, Canada," by Hallie Coltin et al, was published Jan. 25, 2023 in Journal of Clinical Oncology . Funding was provided the Garron Family Cancer Centre Research, the Charles Bruneau Foundation, the National Institutes of Health, the Pediatric Brain Tumor Foundation, the Canadian Institutes for Health Research, the C.R. Younger Foundation, the Canadian Cancer Society Research Institute, Brain Canada, the Rally Foundation for Childhood Cancer, a Canada Research Chair in Pediatric Neuro-Oncology and also by the Ontario Ministry of Health and the Ministry of Long-Term Care.
Media relations: relations.medias.hsj(at)ssss.gouv.qc.ca
About CHU Sainte-Justine
The Sainte-Justine university hospital centre (CHU Sainte-Justine) is the largest mother-child centre in Canada and the second largest pediatric hospital in North America. A member of the Université de Montréal extended network of excellence in healthcare (RUIS), Sainte-Justine has 5,457 employees, including 1,532 nurses and nursing assistants; 1,000 other healthcare professionals; 520 physicians, dentists and pharmacists; 822 residents; and more than 204 researchers, 411 volunteers and 4,416 interns and students in a wide range of disciplines. Sainte-Justine has 484 beds, including 67 at the Centre de réadaptation Marie Enfant, the only exclusively pediatric rehabilitation centre in Quebec. The World Health Organization has recognized CHU Sainte-Justine as a "health promoting hospital."